Hmmm, struggling with infertility...
You can call it a vicious cycle. You can say it’s a which-came-first-the-chicken-or-the-egg situation. But the fact of the matter is that stress can be a cause of infertility.
And infertility causes stress.
And no one telling you to “just relax” is the solution, that’s for sure.
It’s awful to know that your stress can be affecting your fertility because, of course, that’s just going to stress you out more. But if we break down the whys and the hows of the stress-infertility connection, it can help us better understand what to do about it.
Understanding Hormones and the Menstrual Cycle
Before we look at stress, it’s vital to have a general understanding of the menstrual cycle and the key hormones involved. This is because of how hormones are impacted by stress.
As most women know from their own personal experience and those of other women in our lives, everyone’s cycle is different. Usually, this cycle lasts anywhere from 21 to 40 days, although 24 to 38 days tends to be more typical.
Ignore the fact that many sources will depict a cycle as 28 days and act like consistency in the length is the only way to be healthy. We know the truth is that every body is different and so is every experience.
The cycle begins as menstruation starts, shedding the lining of the uterus that is not needed if there is no pregnancy. At this point, both progesterone and estrogen are at their lowest.
The low hormone levels trigger the brain’s pituitary gland to release follicle-stimulating hormone (FSH), causing an egg in the ovarian follicle to start to mature.
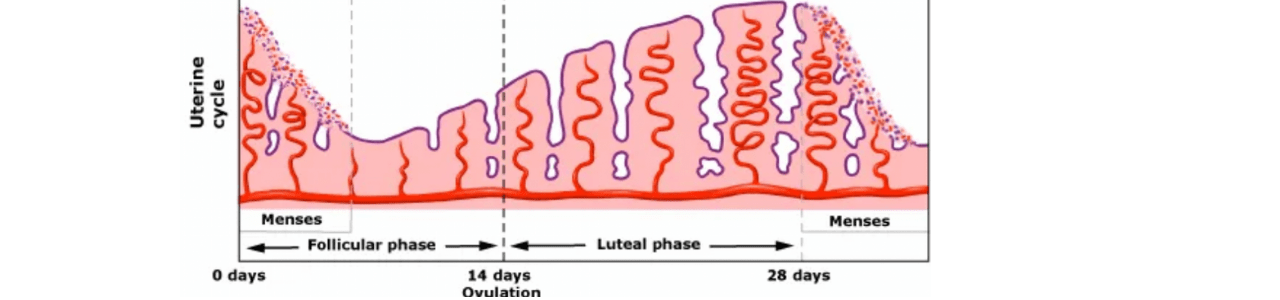
As the egg matures, estrogen begins to be released by the ovary. This estrogen tells the pituitary gland to signal the production of luteinizing hormone (LH), causing ovulation, or the release of the egg. Estrogen is now at its highest in the cycle.
The used follicle, called a corpus luteum, now releases progesterone and, to a smaller degree, more estrogen.
The progesterone causes the uterus to begin to build up the lining that will house and protect the egg once it reaches the uterus. Progesterone is at its highest just before the uterine lining is at its thickest.
As the corpus luteum starts to break down, it produces less hormones, which continue to decline toward the end of the cycle.
If the egg is not fertilized, the lining is no longer necessary and will start to shed again, starting the cycle all over.
You can see from this that hormones play a very crucial role throughout the process. And any interruption of those hormones can greatly impact how it all plays out.

The Relationship Between Sex Hormones and Stress Hormones
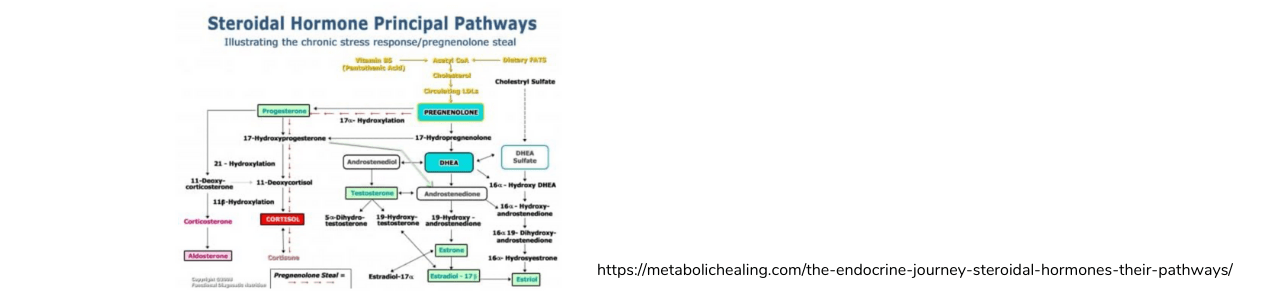
Despite how it is often villainized, cholesterol is actually the back bone for a number of steroid hormones. (I like to think of cholesterol and “Mother Hormone.”) Cholesterol is converted into whatever hormones the body needs most at that moment.
First, cholesterol is converted into pregnenolone. Then, depending on what is being prioritized by the body, pregnenolone is converted to progesterone or DHEA.
DHEA is a precursor for both testosterone and estrogen. But progesterone can become cortisol, one of the most important stress hormones. In fact, progesterone can be bypassed in favor of making cortisol, so that very little progesterone is actually produced (more on this in a bit).
Adrenaline is the stress hormone for short-term stress, think of our ancestors being chased by saber tooth tigers. Cortisol is the long-term stress hormone. In this case, think of our ancestors going through times of drought and famine, when food might be scarce for months on end.
It is cortisol that stays at high levels when we have stressful jobs, daily traffic and money problems that loom.
In these times of stress, our body is more likely to prioritize creating cortisol instead of sex hormones.
Cortisol has also been found to inhibit gonadotropin-releasing hormone (GnRH), which is what triggers the pituitary gland’s release of LH.

Living in Fight-or-Flight Affects Fertility
If you aren’t familiar with the terms sympathetic and parasympathetic modes, you may be aware of their more casual names: fight-or-flight and rest-and-digest, respectively.
Parasympathetic mode, also known as rest-and-digest, is the mode of the nervous system that we are in when we are calm and not stressed out. During this time, our bodies are allowed to focus on proper and healthy digestion, meaning they can better break down food and absorb nutrients. We have better and more consistent bowel movements in this mode.
Our bodies can also focus on reproducing.
But when we are in sympathetic mode, aka fight-or-flight, all we are focusing on is survival. Digestion and reproduction are secondary in that moment.
Because when we’re running from the saber tooth tiger, making babies is not a priority.

And this is not necessarily a bad thing. Stress allows us to survive. But not necessarily thrive, especially long-term.
In fact, cortisol is highly inflammatory.
And as we’ve learned, it also “steals” our sex hormones - as mentioned above - the production of progesterone can be bypassed in favor of making cortisol, so that very little progesterone is actually produced. And, remember, progesterone supports fertility.
Ok, ready for some examples of this in real life?
Menstrual Cycle Under Stress
Let’s review each step of the menstrual cycle and look at how stress, and specifically cortisol, affects them.
Here we go...
Imagine your menstruation is over and your estrogen and progesterone levels are low (as they should be at this point). But you’ve had a bad week at work, the holidays are coming up, the house is a mess and you have no idea what’s for dinner.
Instead of your estrogen levels starting to rise, your body has used that cholesterol to create cortisol. Estrogen may still be created but at lower levels than usual, so the pituitary gland isn’t triggered. Or, if it is, cortisol additionally blocks the release of LH via the GnRH. The follicle isn’t triggered to release the egg, or it is released later than usual, throwing off your usual cycle.
As the stress continues, progesterone that should be released next is instead converted into more cortisol. Without adequate progesterone, your uterine living isn’t building up enough or in time to support the growth of a fertilized egg.
SUMMARY: High stress levels - and therefore your body’s need for cortisol to deal with that stress - has affected your chances for pregnancy in two different stages of your cycle.
Additional Ways Stress Impacts Fertility
Women aren’t the only ones affected by stress in ways that may prevent pregnancy. When men are under stress, they too need cortisol, taking it away from testosterone production.
This has a huge effect on sperm count and quality, as well as being a leading cause of erectile dysfunction and low libido.
Both men and women can experience stress affecting lifestyle and choices they make that are factors in fertility.
Stress can influence sleep, eating habits, exercise consistency, interest in sex, and drinking and caffeine intake. These can all be pieces of the puzzle when struggling with infertility.

How You Can Manage Stress, Not Avoid It
There is nothing that irritates me more than someone telling a woman struggling with infertility to not stress about it. For real.
First of all, if you’ve been struggling with trying to get pregnant (and I don’t care how long because when you want a baby, any wait feels too long), the idea of being able to just let go of that stress is laughable.
It also does not give someone the tools to manage their stress, only acts like they have the ability to remove stressors from their life.
The truth is that money problems don’t just disappear; that traffic will not clear up magically; you will still have nights when you burn dinner; the list goes on and on.
If we had the ability to remove what stresses us out, no one would be stressed. But that is far from the world we live in.
Instead, we need to be talking about how to manage the feelings of stress.
And to make things more difficult, what works may be different for everyone. And what works one day may not work the next.
These are some stress management techniques that work well for some people:
- Breathing exercises
- Yoga
- Massage/body work
- Meditation or guided imagery
- Journaling
- Talk therapy
- Social media breaks
- Cutting back or eliminating caffeine
- Cutting back or eliminating alcohol
- Exercise
- Walk or run
- Nature
- Aromatherapy
- Art or art therapy
- Music, dancing
- Spending time with family or friends (as long as this doesn’t increase stress, catch my drift?)
- Hugs
- Pets
Stress as an Infertility Piece of the Puzzle
For better or worse, there is no one thing that causes infertility.
But there is no denying that stress plays a role in it.
If you have struggled trying to conceive, you probably have already stressed about it and I certainly don’t want to add to that stress. But if you do think it may be a factor in your struggles, there are ways to manage it.
The great news is that most forms of stress management are quite enjoyable. (That is the idea after all.)
Remember to try what appeals to you at that time, knowing that it may help you relax one day but not the next. It is important to prioritize the time you need to make that happen, even if it means asking for help.
The next time someone tells you not to stress may just be the perfect time for that calming breathing exercise.

Whether it’s infertility, autoimmunity or general health support, if you need nutrition therapy that is tailored to you and your lifestyle, my Happy & Healthy Adult Program will have you feeling better than you have in a long time. This is the right fit for you if you already know that underlying health issues, stress patterns or hormonal imbalances are part of the picture.
It’s the perfect place to start if you haven’t worked with me before and don’t know how to begin making changes to your nutrition and your life.