“My hormones are raging!”
“I’m so hormonal!”
We often talk about hormones like...
a) all hormones are sex hormones
b) we have no control over them

The truth is ...
a) there are many kinds of hormones that are impacted by each other
b) there is a lot we can do to balance our hormones
And when it comes to controlling our weight, hormones play a big part, which means that balancing them can make it easier to lose or maintain weight.
This is especially important if you have Hashimoto’s disease, because this autoimmune disorder is known to cause weight gain and impact metabolism.
How Hormones Affect Us and Other Hormones
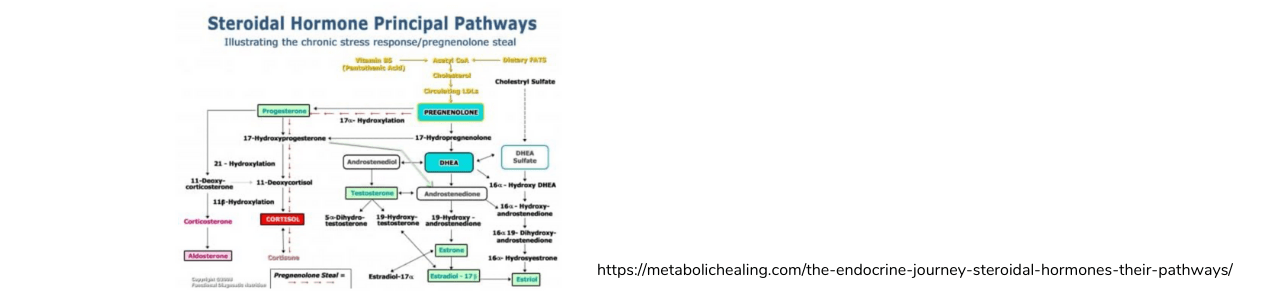
The hormones that are constantly coursing through our bodies are products of different systems in our bodies but affect each other in miraculous ways.
This is because hormones are all produced by the endocrine system and used throughout the body. So, for example, if dysregulation occurs and one hormone is overproduced, it means other hormones may not be made in adequate numbers.
In addition, it is possible to build up a resistance to certain hormones, most famously insulin, which results in diabetes.

There are a number of hormones that affect our hunger, feeling full, our blood sugar and even how we store fat, so these are often referred to as weight loss hormones. There are a number of ways these can be affected by aging, stress, diet, autoimmune disease and much more so that we may be more likely to gain weight or struggle to lose weight.
A Basic Introduction to Weight Loss Hormones
Ghrelin
Ghrelin is often called the “hunger hormone,” is mostly made by the stomach and small intestines and is released when the stomach is empty. It sends a message to the pituitary gland that the stomach needs food, causing you to feel hungry.
Ghrelin levels should be at their lowest after eating.
In people who are obese however, it has been found that ghrelin levels don’t decrease as much after eating, causing them to continue to eat even once hunger should have subsided.
Ghrelin also triggers the release of growth hormone by the pituitary gland and promotes the storage of fat. It may also play a role in insulin release.
There is interest in how lowering ghrelin levels could support weight loss by lessening hunger and appetite.

Leptin
In some ways, leptin could be considered the anti-ghrelin as it is called the “satiety hormone.” Leptin is made in the fat cells and, when triggered, tells the hypothalamus gland that you are full.
Obese people have been found to have high levels in leptin but are more likely to suffer from leptin resistance, in which the brain no longer responds to the secreted hormone.
Studies have found an association in women between high levels of leptin and fewer depressive symptoms.
Insulin
Not many people think about their insulin unless it’s in the context of diabetes. But you don’t have to be diabetic to pay attention to your insulin levels and, in fact, balancing blood sugar is vital for weight management.
When you consume food that contains carbohydrates, the hormone insulin is released to balance the amount of glucose (blood sugar) broken down from the carbohydrates and store any not needed in that moment as fat.
When blood sugar remains elevated for long periods, namely when the diet regularly contains too much sugar and/or simple carbohydrates, it is possible to become resistant to insulin. Then both insulin and blood sugar levels are high, resulting in obesity and diabetes.

Additional Hormones for Weight Gain and Loss
You’ve heard me rail about cortisol before because it is a stress hormone that can cause inflammation and affect fertility. But cortisol may also be impacting your weight in ways you didn’t realize.
First, the inflammation promotes weight gain, especially around the midsection.
Second, you are more likely to overeat and make poor dietary choices when you are stressed. And lastly, increased sugar intake is associated with high stress levels.
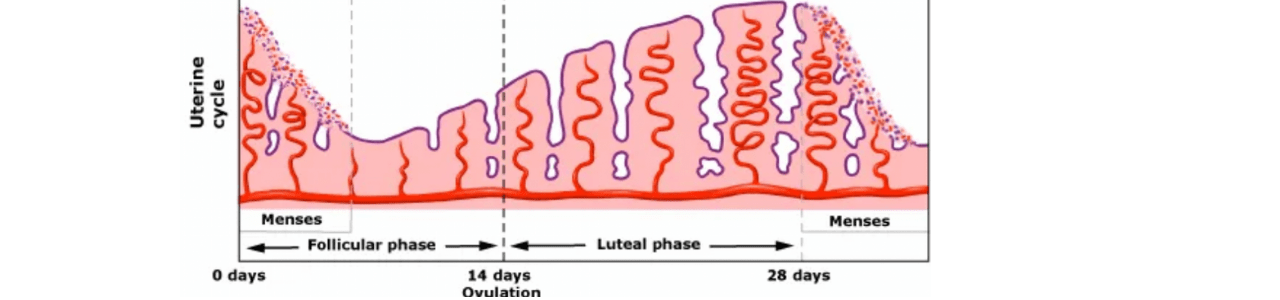
Estrogen is another hormone that we may not directly associate with weight gain but can affect how well you manage your weight.
In order to prepare for possible pregnancy, estrogen levels increase starting in reproductive years, which promotes fat storage. But too little estrogen can also lead to weight gain.
Later I’ll get more into estrogen and how menopause can cause weight changes.
The Big One for Hashimoto’s: Thyroid Hormones
Depending on your base knowledge of Hashimoto’s, you probably understand that it is an autoimmune disease, which means the immune system is attacking your own body, or specifically some aspect of your body.
Hashimoto’s disease is when the immune system attacks the thyroid, a gland located in the neck. When attacked, the thyroid can’t adequately do its job, namely making thyroid hormones.
READ: Your Complete Guide to Understanding Hashimoto’s, Hypothyroidism & Thyroid Testing
Among the many jobs of thyroid hormones is to regulate metabolism, or how quickly and well food is converted into energy (calories), as well as how quickly and well you use those calories. Low thyroid hormones means slow metabolism means weight gain.
So naturally, people with Hashimoto’s are more at risk for weight gain.
In addition, insulin resistance increases your risk of autoimmune disorders like Hashimoto’s, so you may be struggling two-fold.
How Age Affects Hormones Levels and Weight
Once you understand the role hormones play in weight management, it will come as no surprise that different phases of life can bring up hormonal changes that affect weight.
Although anyone can experience a change in metabolism as they age, women are especially susceptible to this, partially because of the role estrogen plays and because women are more at risk for Hashimoto’s.
In general, as you age, you are more prone to nutrient deficiencies because your stomach acid decreases, which affects both the breakdown of food and absorption of nutrients.
This decline of nutrients affects a number of bodily functions, including metabolism.
The risk of insulin resistance increases in your 40s, and this can also be the age when some people start to notice new food sensitivities, which increases inflammation.

While women can experience their first glimpse of menopause at different ages, it is most common to have this process start in your 50s.
If you remember, very high or very low levels of estrogen can both cause weight to go up. And menopause can cause estrogen levels to plummet, leading to weight gain.
READ: Menopause Makes Hashimoto’s Worse! But, Nutrition Can Help!
The Good and Bads News About Hormonal Weight Changes
Here’s the part you may have skipped ahead to: The part where I tell you what single, magic supplement you can take to effortlessly lose weight.
Um, just kidding, that magic supplement for weight loss simply does not exist.
Now that you understand some of the hormones that may be standing in the way of your ideal weight, you may think you can just supplement with some leptin or something. But of course it’s never that easy.

As I’ve said, these hormones work together in a complex system, or really systems, that need to be in balance with each other.
But the really good news is that there are ways that you can boost certain hormones and keep others lower, just by eating certain foods and avoiding others.
And even better, many of the same steps will affect more than one hormone, offering a double-whammy of sorts.
Nutrition to the Rescue!
Get Plenty of Protein
One way you can balance both hormones and blood sugar is to make sure to get your share of protein with every meal. It doesn’t take a ton but including protein (whether from animal sources like meat and eggs, or from vegetarian sources like beans and nuts) reduces:
- Insulin resistance in the long-term
- Ghrelin levels and makes you feel full longer
- Neuropeptide Y (NPY), another appetite-stimulating hormone

Reduce Sugar and Simple Carbohydrates
Sugar, high-fructose corn syrup and artificial sweeteners not only cause blood sugar spikes and therefore a sharp increase in insulin, they can prevent the natural ghrelin response after eating, allowing you to overeat.
This goes for simple carbohydrates as well. These are grains that have been processed to eliminate beneficial components of carbohydrates, such as fiber. Without this, the carbohydrates are more quickly converted to glucose.
Making sure you get plenty of fiber has the added benefit of assisting the body in flushing out excess estrogen when it is too high. Insoluble fiber (found in nuts, seeds, whole grains, fruit skin and fibrous vegetables) works as a prebiotic to feed gut bacteria, which helps lower NPY levels.

Eat Healthy Fats Every Day
Healthy fats like omega-3 fatty acids from fish or flax seeds, medium-chain triglycerides from coconut oil and monounsaturated fats from nuts all help increase insulin sensitivity and trigger satiety.
But not all fats are created equal. Trans fats have the opposite effect, decreasing insulin sensitivity and promoting fat storage around the middle.
Know that Cruciferous Vegetables are Your Friends
Whether you roast some cauliflower, steam some broccoli, air fry some Brussels sprouts, saute some cabbage or munch on raw kale, cruciferous vegetables are your best friend if you’re aiming to lose weight.
Cruciferous vegetables are high in fiber, balance estrogen levels and naturally detoxify pro-inflammatory toxins.
Make Lifestyle Choices for Balanced Hormones
In addition to nutrition changes, lifestyle changes can also have a big impact on hormones and therefore weight.
Ok, I’ll start with the obvious: exercise. But not just for the reasons you think. Yes, exercise can burn fat and build muscle. But it also helps with insulin sensitivity while also lowering insulin levels. It also improves leptin sensitivity and levels out estrogen levels.

Depending on the kind of exercise, it can also help you manage stress and lower cortisol levels.
Be careful, though, as too much exercise, or the wrong kind of exercise, if you are duly struggling with some low adrenal function can make things worse. So, in order to know what you're up against, get proper testing.
Also helping with stress is sleep. Getting enough sleep can raise leptin levels, lower ghrelin levels and allows you to make better choices about your diet. (Lack of sleep has been proven to increase cravings and reduce will power.)
Looking for a Guided Approach to Balancing Hormones and Losing Weight?
I know from my own experience that when you have Hashimoto's, the weight loss or weight management struggle is real. And, sometimes, when you feel exhausted, weak, or unmotivated, doing even the simplest things to help your body can feel overwhelming.
Sometimes you need a helping hand.
If you want to learn about how Hashimoto’s, general hormone balance and weight management is interrelated AND improve your total health - working with me one-on-one can provide the most clarity.
You can also check out my Happy & Healthy Adult Program – designed for individuals with Hashimoto’s (and also hormone imbalance or chronic weight issues) looking for a personalized, sustainable and joyful approach to nutrition and lifestyle measures which can help heal your body.

I am here to help!